It can lead to future new treatment strategies for type 2 diabetes. A scientific challenge is to explain how a cell/organ can, at the same time, be resistant in a biological function to insulin and insulin sensitive in another.
Insulin insensitivity, also called insulin resistance, is associated with type 2 diabetes and affects various types of cells and organs in the body.Now, scientists from the Karolinska Institute, in Sweden, have discovered a mechanism that explains how insulin producing cells can be resistant to insulin and insulin sensitive at the same time, a finding that is published in the magazine 'Cell Reports' andwhich can lead to future new treatment strategies for type 2 diabetes.
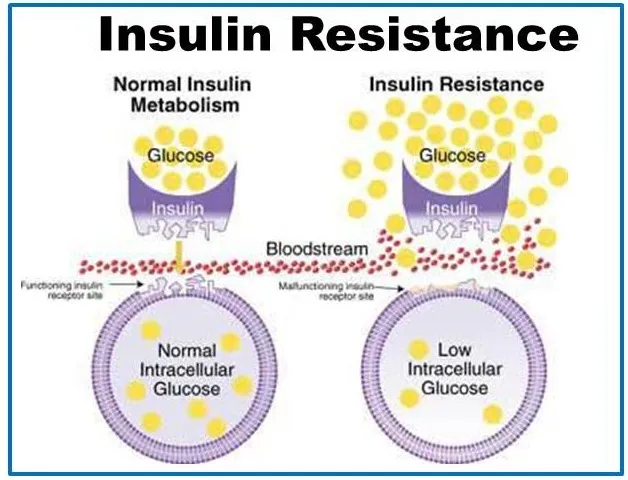
Insulin is critical in reducing blood glucose concentration.People with type 2 diabetes suffer from insulin resistance and this means that their cells/organs are insensitive to insulin, which their body tries to compensate producing more insulin and also raising the number of insulin producing cells.Finding new treatment strategies is only possible with a greater understanding of what happens in the body of a diabetic patient.
A scientific challenge is to explain how a cell/organ can, at the same time, be resistant in a biological function to insulin and insulin sensitive in another.The Barbara Leibiger and Ingiger doctors, both members of the Research Group of Professor Per-Olof Berggren, in the Department of Medicine and Molecular Surgery of the Karolinska Institute, are particularly interested in the beta cells of insulin producers.
"The beta cell must have insulin to work properly," says Barbara Leibiger, associate teacher and main author of the current study.In a person with diabetes, beta cells become insensitive to insulin. ”Researchers have previously demonstrated that the beta cell has two receptors with different biological functions, insulin A and insulin B receptor B.
In the current study, the authors detected that under diabetic conditions, despite the fact that insulin B receptor is insensitive to insulin for a signaling route, insulin can under these conditions activate a different signaling route, giving rise to theBeta cell proliferation.The researchers also identified the PI3K-C2A factor, which caused the change from one signaling route to another.
"The results are important, since they explain how the beta cell can go from a differentiated state to a proliferative state," says Ingo Leibiger, who cosupervised the study with Professor Berggren."This means that cells change from being glucose to increase in number," he adds.
According to the team, which also has Korea experts, the factors involved in the change of the insulin signal represent possible therapeutic targets in the treatment of diabetes.