Researchers at Harvard University in Boston (USA) have managed to create 'mini-stomachs' of reprogrammed cells of the mice pylorus that, once transplanted, have the ability to produce insulin to correct the high levels of blood glucose.That is, with the ability to treat diabetes.
Specifically, the study, published in the "Cell Stem Cell" magazine, shows how pylorus cells can be reprogrammed in insulin producing cells and, subsequently, joining forming spheres-or 'mini-stomachs'-that after being transplanted they are capableto control glucose levels.
More;Since these ‘mini-stomachs’ also contain pylorus stem cells, have the ability to regenerate continuously, which guarantees an unlimited presence of insulin producing cells to treat diabetes.Or so, at least, in mice.
The first step of the study was to identify the mouse organism cells that have greater ease to be reprogrammed in insulin producing cells.And in order to further facilitate this step, the authors used genetically modified animals to express three genes capable of transforming any cell into a beta cell of pancreatic islets - the cells responsible for insulin production in the body.
As explained by Qiao Zhou, director of the study, «in our study we analyze all mouse cells, from the nose to the tail.And surprisingly, we discover that pylorus cells are the most likely for their conversion into beta cells.Thus, this fabric was shown as the most suitable to start our work ».
Specifically, the pylorus is the stomach region linked to the small intestine.And once reprogrammed, pylorus cells are those that offer a greater response when exposed to high insulin levels.Or otherwise, they are the type of cell with the greatest capacity to produce insulin and, thus, normalize blood glucose levels in mice.
We can get a person's cells, grow them in vitro, reprogram them in beta cells and transplant them to offer a therapy for each patient.
Thus, and in order to evaluate the viability of their reprogrammed pylorus cells, the authors destroyed the pancreatic islets of the mice.The result is that those mice to which these reprogrammed cells had not been transplanted did not survive beyond eight weeks.On the contrary, animals that benefited from this ‘transplant’ maintained normal blood glucose levels, so they did not die during the study monitoring period - how duration it exceeded six months.
But, in addition, the pylorus presents an added advantage.And, in natural conditions, their stem cells are responsible for regenerating stomach tissue in a continuous way.In fact, the study showed that when reprogrammed cells are destroyed, stem cells contained in transplanted grafts themselves are capable of generating new insulin producing cells.
As highlighted by qiao zhou, «patients experience a constant loss of beta cells during the different stages of the disease.And, at least in principle, our study offers the advantage of replacing the loss of these cells ».
At this point, the question that arises is how to transfer the results to clinical practice.As he recognizes qiao zhou, «in our study we activated the three genes once the mice had reached adulthood.However, and weighing in clinical terms, we cannot develop transgenic humans ».
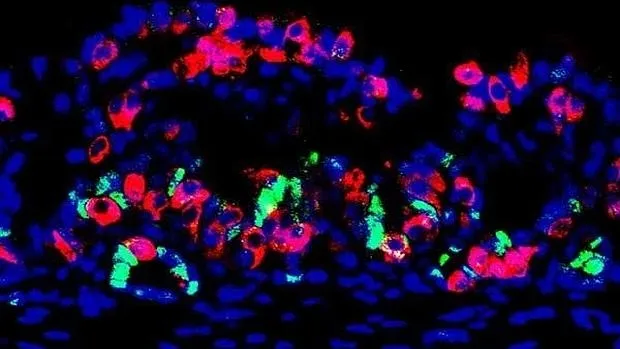
In order to solve this problem, the researchers took pylorus cells, theThey rescheduled in beta cells and forced them to grow forming spheres-or ‘mini-stomachs’-with the ability to produce insulin and regenerate from their stem cells.Thus, and once the ‘mini-stomachs’ developed, they were transplanted in the abdominal membrane of the mice.
And these ‘mini-stomachs’ are functional?Well, to find out, the authors destroy the pancreatic islets of the mice.And what they saw is that the ‘mini-stomachs’ were able to compensate for the insulin produced by beta cells now destroyed in 5 of the 22 mice, so blood glucose levels remained normal.
As it concludes that Zhou, “which is potentially remarkable from our study is that cells can be obtained from a biopsy of any person, growing these in vitro cells and reprogramming them in beta cells, and then transplanting them to offer a specific therapy for each patient.And this is those that we are worked at at this time ».