Bone fractures in diabetic experimental models heal better in the presence of a protein that stimulates the activity of skeletal stem cells, according to a study conducted by researchers at the Faculty of Medicine at Stanford University, in Palo Alto, California, United States, and published in 'Science Translational Medicine'.
The protein counteracts a decrease in the activity of the stem cells that the researchers observed both in diabetes mouse models and in bone samples of diabetic patients who had been subjected to joint replacements.The authors expect the discovery to lead to ways to help people with diabetes to heal the broken bones more efficiently.
"We have discovered the reason why some diabetes patients do not heal well from fractures and we have found a solution that can be applied locally during surgery to repair the break," says the director of the Stanford Institute of Biology of stem cells and stem cells andRegenerative medicine, Michael Longaker."Diabetes is unbridled worldwide and any improvement in the ability of affected people to cure fractures could have a greatly positive effect on their quality of life," he adds.
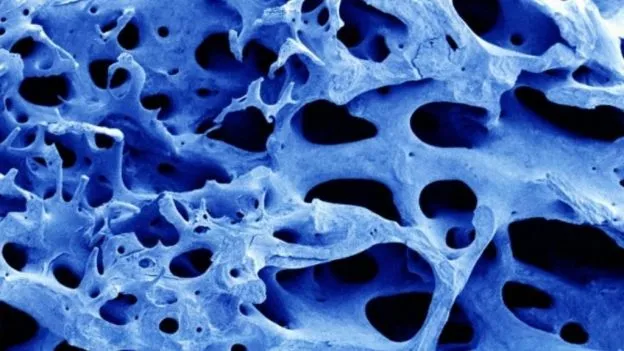
Diabetes mellitus is a metabolic disease characterized by the inability to produce or respond properly to insulin;It affects hundreds of millions of people worldwide and their prevalence is increasing.In addition to causing dangerous oscillations in blood sugar levels after meals, the disease leads to many other weakening symptoms, such as decreased ability to cure soft tissue injuries and skeleton fractures, but the precise molecular reason is unknownof this alteration of bone healing.
Longaker, professor of plastic and reconstructive surgery, and co -authors Charles Chan, a researcher at the stem cell institute, and Ruth Tevlin, postdoctoral researcher, are based on previous works on which they and colleagues of the laboratory of the author Irving Weissman, teacher ofPathology and biology of development, identified and described a population of cells in mice bones that serve as skeletal stem cells (SSC).
These adult stem cells can become all components of the skeletal system, including bone, cartilage and a part of the bone marrow known as stroma.Subsequently, these experts showed that the healing of fractures in mice is severely affected when these stem cells are exhausted, a finding that made them think.
"We wanted to apply what we knew about skeletal stem cells to the problem of bone healing deficiency in people with diabetes," does the disease affect the cure of the fracture in some way by modulating the activity of thesestem cells? "
The researchers used a type 2 diabetes mouse model, in which the disease arises when animals are about four weeks.Before the development of the disease, the prediabetic mice were able to cure the fractures of the bones of the legs as effectively as the wild type rodents, the researchers saw.
In contrast, after the disease had manifested, the repaired bone was significantly weaker and less dense than the bone in control animals.When they compared the number of SSCs in the healing bone seven days after the fracture, they found that diabetic rodents had significantly lower amounts of these cells than control animals.
Signaling problems
A series of experiments ruled out a reasonSystemic for this reduction in the number of stem cells and confirmed that the cells themselves were totally functional, which left only a possible problem with the signals that the cells were receiving from the surrounding environment, or the place.When Tevlin and his colleagues analyzed that environment, they saw that diabetic animals produced significantly lower levels of a family of signaling proteins called Hedgehog that is known to play a critical role in many biological processes, such as embryonic development and tissue regeneration.
The researchers collaborated with Co -author Philip Beachy, professor of biochemistry and development biology, to test whether the artificial blockade of the Hedgehog signaling path could harm bone healing in non -diabetic mice.In this way, they found that in the control mice exposed to a molecule that blocked this route the bones recovered were weaker and more fragile, as in diabetic animals.
"Then, we had to prove if adding Hedgehog signaling proteins again in the local environment in diabetic animals restored their ability to cure fractures," Longaker explains.The researchers collaborated with the Co -authors Fan Yang, assistant professor of bioengineering and orthopedic surgery, and the postdoctoral scientist Xinming Tong, to design a biologically friendly hydrogel in which the Hedgehog signaling proteins were embedded and the gel was applied directly to the fracture site."And these animals healed like normal mice," says Longaker.
Finally, the team contacted the co -author Stuart Goodman, an orthopedic surgery professor, to obtain bone samples of patients with diabetes who were subjected to replacement of joints for osteoarthritis.They compared the expression of important proteins for the Hedgehog signaling route of these samples with other non -diabetic patients.
Normally this fabric would be discarded by the surgeon, but in this case it contained important clues."What we saw in these human samples was a reflection of what we saw in the mice-Subraya Chan-. The bones of diabetic patients showed a significant reduction in the expression of these important signaling proteins."
Longaker, Chan and Tevlin believe that the inhibition of the Hedgehog signaling route arises from the inflammation associated with diabetes that causes high levels of a molecule called tumor necrosis factor Alfa (TNF-alpha).It is known that TNF-ALFA levels are high in diabetes and researchers observed a corresponding increase in their disease mouse models.
They also discovered that these increased levels of TNF-Alfa inhibited the expression of some members of the Hedgehog family.However, the direct inhibition of all the activity of the TNF-Alpha could have other dire consequences for an animal or a human patient because TNF-Alpha plays many important biological roles.
"We have devised a feasible strategy to reverse a specific pathology of the tissue-the inability to cure skeletal fractures efficiently-in a complex metabolic disease such as diabetes through the local application of a compound to stimulate the activity of adult stem cells,", summarizes Longaker.