Glycosylated hemoglobin (HBA1C) is used almost universally to help doctors in the diagnosis of type 2 diabetes. However, a new study published in 'Diabetology' and conducted by experts from the University of Nottingham, in the United Kingdom,Relief how anemia, a common disorder in the general population, especially in women, can lead to a false diabetes diagnosis based on HBA1C, when a person's blood sugar control is actually normal.
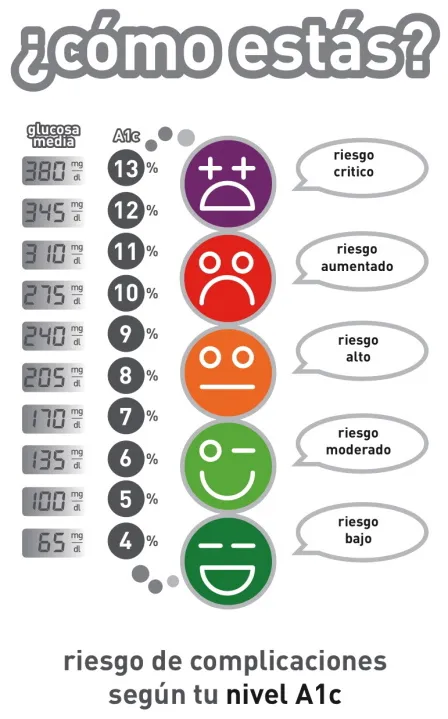
In recent years, there has been a movement towards the use of HBA1C for the diagnosis of type 2 diabetes (T2D).The World Health Organization (WHO) and the American Diabetes Association (AD) have defended the use of HBA1C for the diagnosis of this disease, with a value of 6.5 percent (48 mmol/mol).In the United Kingdom and most of Europe, the same cutting point is used.
Following WHO recommendations to use HBA1C as a diagnostic method for type 2 diabetes, the United Kingdom (through the Department of Health of its Government) issued a scientific advice that indicates that one of the main problems that affect this technique isAnemia, modifying hemoglobin levels (HB) in the blood.
WHO defines anemia in adults such as 120 g/l of HB in non -pregnant women and 130 g/l in men.With approximately 29% percent of non -pregnant women worldwide anemia (last estimation of 2011), this translates into a significant number of people in which the use of HBA1C for the diagnosis of diabetes does notIt is suitable.The latest WHO estimate for the prevalence of anemia in men was 13 percent, probably higher in elderly men, although the data is scarce.
In this systematic review, the authors intend to address the above issues through the evaluation of the available evidence on the impact of the alterations of the erythrocyte indices (red blood cells) and the anemia in the HBA1C levels on the 48 mmol mmol cutting point/mol (6.5 percent) for the diagnosis of WHO/ADA.
The review of the research between 1990 and 2014 included studies that had at least one measurement of HBA1C and glucose and at least one anemia index in adults, excluding pregnant women and diagnosed with diabetes.The authors identified 12 appropriate analysis to include them in their work, most focused on iron deficiency anemia and, in general, demonstrated that the presence of iron deficiency with or without anemia led to an increase in HBA1C values inComparison with controls, without increased blood glucose, thus making a diagnosis of diabetes in these unreliable individuals without further evidence.
The authors explain: "HBA1C can be affected by iron deficiency and iron deficiency anemia, with a spurious increase in HBA1C values. This can lead to confusion in the diagnosis of diabetes through HBA1C. This reviewClearly identify the need for more evidence, especially in the identification of the types and degrees of anemia that are likely to have a significant impact on the reliability of HBA1C ".
While more evidence is collected, the authors make several recommendations in relation to clinical practice.For example, they advise that anomalies related to anemia or iron deficiency are considered during the monitoring of people with diabetes, when glucose and HBA1C levels give different results
Iron deficiency, as well as iron deficiency anemia, can be enough to cause a change in HBA1C values;something of great relevance in women of childbearing age,According to these experts.They also propose to take into account the correction of anomalies such as anemia, for example with iron supplements, before using HBA1C for diagnosis.
Studies included in this review suggest that it can cost up to six months after treatment normalize hemoglobin levels."The key questions that have not yet been answered are whether anemia and anomalies in red blood cells will have a significant impact on the diagnosis of diabetes through HBA1C in the general population, something that is now widely used," conclude the authors.